FODMAP Diet: What You Need to Know, Foods to Eat & Avoid
April 30, 2025

The Ultimate Guide to the Low FODMAP Diet: What to Eat, Avoid, and How to Find Relief from IBS and SIBO
What is the FODMAP Diet?
The FODMAP Diet was developed in 2005 by researchers at Monash University in Australia as a way to help manage digestive symptoms, particularly for individuals with Irritable Bowel Syndrome (IBS) or inflammatory bowel disease (IBD).FODMAPs are specific types of short-chain carbohydrates that are poorly absorbed in the small intestine. For many people, consuming foods high in FODMAPs can lead to symptoms like bloating, gas, diarrhea, constipation, and abdominal pain.
What Does FODMAP Stand For?
FODMAP is an acronym that represents:
- Fermentable – Quickly fermented by gut bacteria
- Oligosaccharides – Found in wheat, rye, legumes, garlic, onions, and artichokes
- Disaccharides – Mainly lactose, found in milk, yogurt, and soft cheeses
- Monosaccharides – Fructose, found in honey, apples, and foods with high-fructose corn syrup
- And Polyols – Sugar alcohols like sorbitol and mannitol, found in certain fruits, vegetables, and sugar-free products
These sugars can draw water into the intestines, leading to bloating and diarrhea, and ferment in the colon, causing gas and digestive discomfort.

Common high FODMAP foods to avoid if you’re following a Low FODMAP Diet as these can trigger digestive issues in people with IBS or SIBO.
What is the Low FODMAP Diet?
The Low FODMAP Diet is a carefully designed eating plan aimed at helping people with IBS and SIBO manage their digestive symptoms. It involves restricting foods high in FODMAPs, allowing the gut to heal, and later reintroducing foods systematically to identify specific triggers.The main goal is to limit short-chain carbohydrates that are difficult to digest and absorb, reducing symptoms and improving quality of life.Important: Always consult a healthcare provider or dietitian before starting a low FODMAP diet to ensure it’s the right approach for you.

Gut-friendly foods you can enjoy on a Low FODMAP Diet; including safe proteins, dairy alternatives, fruits, vegetables, and grains that support IBS and SIBO symptom relief.
Are There Benefits to Following a Low FODMAP Diet?
Absolutely. Studies have shown that following a low FODMAP diet can:
- Reduce abdominal pain, bloating, gas, diarrhea, and constipation
- Improve overall digestive comfort
- Enhance quality of life for those suffering from IBS or SIBO
However, because the diet involves significant food restrictions, it’s crucial to follow it under professional supervision to maintain balanced nutrition across protein, fat, carbohydrates, fiber, vitamins, and minerals.
How the Low FODMAP Diet Works: A 3-Step Process
- Elimination Phase (2–6 Weeks): Completely remove all high-FODMAP foods from your diet. This allows your gut to reset and symptoms to improve. Medical professionals suggest sticking to the elimination phase of the diet for a duration of two to six weeks. This helps alleviate symptoms and, in the case of SIBO, can reduce abnormally high levels of intestinal bacteria.
- Reintroduction Phase (6–8 Weeks): Slowly reintroduce one FODMAP group at a time, every 3 days, to observe any digestive reactions. This step helps identify which specific FODMAPs cause symptoms. If a specific high FODMAP food triggers symptoms, it’s wise to avoid it in the long run.
- Personalization Phase (Ongoing): Once trigger foods are identified, you can personalize your long-term eating plan, minimizing problematic foods while keeping your diet varied, balanced, and enjoyable.
Important Reminders:
- The Low FODMAP Diet is NOT meant for long-term elimination.
- Extended restriction without reintroduction can harm gut health and beneficial bacteria.
- Medical supervision is especially critical for underweight individuals or those with pre-existing health conditions.
Following this structured approach can make the journey smoother, more effective, and nutritionally safe. Keep in mind that dietary restrictions vary for each person based on their health, so it’s crucial to have a direct conversation with your doctor if you’re considering the FODMAP diet.
Symptoms That May Improve on a Low FODMAP Diet
If you experience gut-related symptoms, reducing FODMAPs could bring relief from:
- Gas and bloating
- Abdominal cramping
- Diarrhea
- Constipation
- Excessive flatulence
- Stomach pain
- Abdominal discomfort
- Nutritional stress linked to SIBO
- General digestive distress
📈 Research indicates that up to 86% of IBS patients see noticeable symptom improvement when the Low FODMAP Diet is correctly followed.
Who Should Consider a Low FODMAP Diet?
The Low FODMAP Diet is primarily recommended for:
- Individuals diagnosed with Irritable Bowel Syndrome (IBS)
- Patients with Small Intestinal Bacterial Overgrowth (SIBO)
- People experiencing chronic bloating, gas, or bowel irregularities without an underlying disease
However, it is not suitable for:
- Underweight individuals (due to risk of further weight loss)
- Those with eating disorders (due to restrictive nature)
- People with diagnosed gastrointestinal diseases like Celiac Disease (different dietary needs)
Expert Advice: Why Medical Supervision Matters
Doctors may also recommend combining diet changes with:
- Antibiotics (for SIBO management)
- Laxatives (for constipation-dominant IBS)
- Stress management techniques or low-dose antidepressants
Tips for Success on a Low FODMAP Diet
✅ Plan Ahead: Batch cook meals using low-FODMAP ingredients.
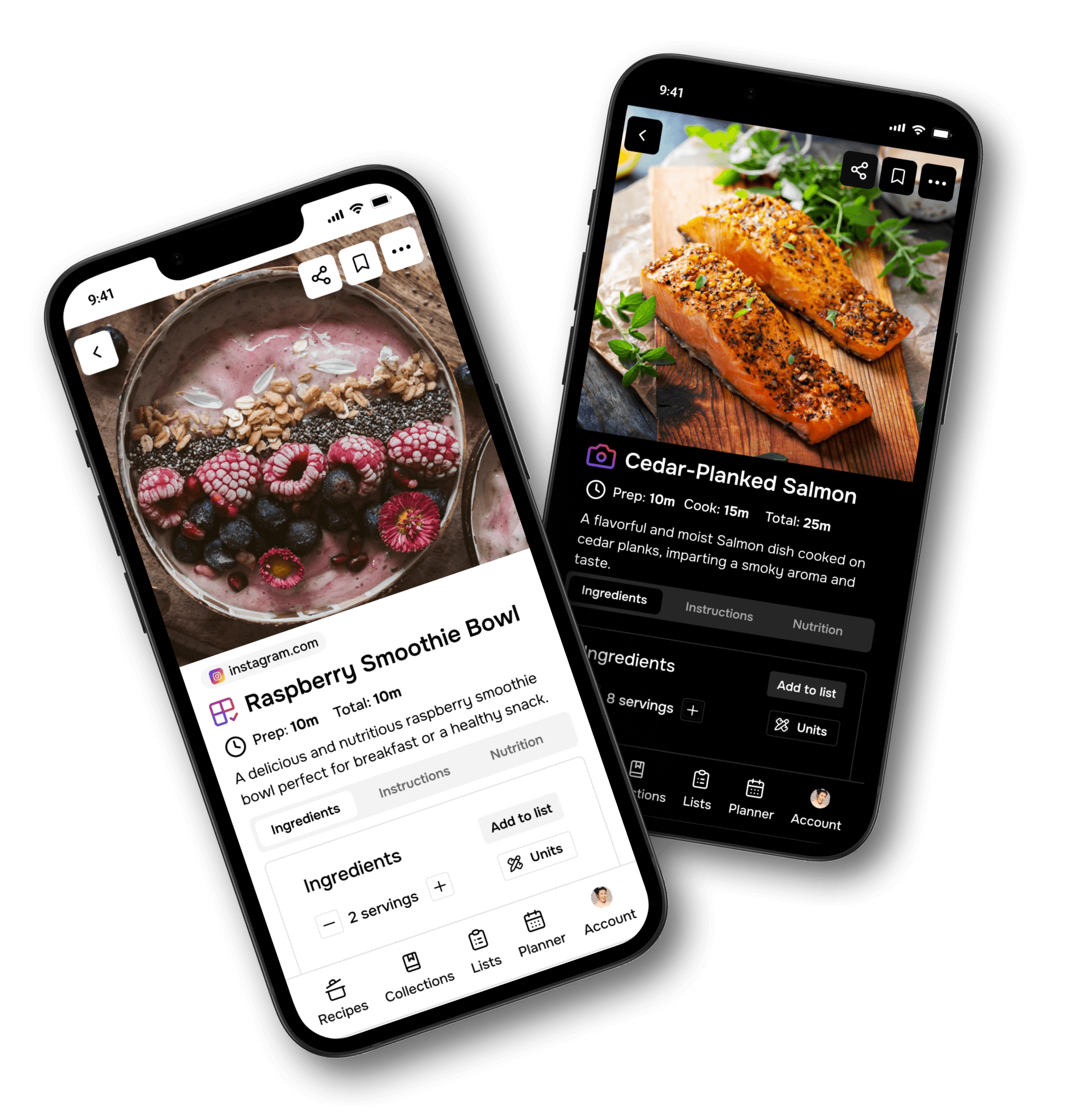
✅ Use Trusted Resources: Apps like Monash University’s FODMAP App offer accurate food lists.
✅ Keep a Symptom Diary: Track what you eat and how you feel to spot patterns.
✅ Focus on Nutrient Density: Choose fiber-rich and calcium-rich low-FODMAP foods to avoid deficiencies.
✅ Reintroduce Foods Carefully: Add back one food at a time during reintroduction for clearer results.
Common FAQs About FODMAPs
How long should I stay on a Low FODMAP Diet?
The elimination phase of the Low FODMAP Diet should last only 2 to 6 weeks, followed by a careful reintroduction of foods to identify your specific triggers. The Low FODMAP Diet is a short-term strategy, not a permanent eating plan. Its goal is to help you discover which FODMAPs your body struggles with, so you can personalize your diet for long-term gut health while maintaining overall nutrition.
What does FODMAP stand for?
FODMAP stands for Fermentable Oligo-, Di-, Mono-Saccharides, and Polyols. These are scientific terms for specific groups of carbohydrates that can trigger digestive symptoms.
What are the symptoms of FODMAP intolerance?
While not everyone reacts to FODMAPs, sensitive individuals may experience, but for some folks, they might bring on cramps, bloating, gas, or diarrhea. These symptoms occur because FODMAPs draw water into the gut and ferment rapidly, producing gas and irritation.
Is a Low FODMAP Diet the same as a gluten-free diet?
Not exactly. Although wheat (which contains gluten) is restricted on a Low FODMAP Diet due to its fructan content, gluten itself isn’t the issue. Low-FODMAP plans can still include some gluten-containing foods like sourdough spelt bread if they are low in FODMAPs.
Do I have to give up dairy on a Low FODMAP Diet?
Only lactose-containing dairy needs to be restricted. You can still enjoy lactose-free products and low-lactose options like hard cheeses (e.g., cheddar, parmesan).
Does the Low FODMAP Diet cure IBS?
No, the Low FODMAP Diet does not cure IBS. However, studies show that 70% to 86% of people with IBS experience significant symptom improvement when following the Low FODMAP protocol correctly.
Can a Low FODMAP Diet help with SIBO?
Yes! Reducing fermentable carbohydrates can help decrease bacterial overgrowth in the small intestine, relieving many of the uncomfortable symptoms associated with Small Intestinal Bacterial Overgrowth (SIBO).
What's the difference between the Low FODMAP, Gluten-Free, and Dairy-Free Diets?
- The Low FODMAP Diet focuses on limiting specific fermentable carbs to manage digestive symptoms.
- A Gluten-Free Diet eliminates gluten proteins entirely, primarily for people with celiac disease.
- A Dairy-Free Diet removes all dairy products, often used to manage lactose intolerance or milk allergies.
Each diet serves a different purpose and addresses different health needs.
What is Irritable Bowel Syndrome (IBS)?
Irritable Bowel Syndrome (IBS) is a chronic disorder affecting the large intestine, leading to symptoms such as:
- Abdominal pain
- Gas
- Bloating
- Diarrhea
- Constipation IBS is a functional disorder, meaning it affects how the gut works without visible signs of damage.
What are the symptoms of IBS?
Common symptoms of IBS include:
- Cramping and abdominal pain
- Bloating
- Alternating constipation and diarrhea
- Mucus in the stool Managing IBS often requires a combination of dietary changes, lifestyle adjustments, stress reduction, and medical treatments.
- It's important to work closely with a board-certified gastroenterologist for personalized care.
What causes IBS?
The exact cause of IBS remains unclear. However, it’s believed to involve a combination of:
- Gut-brain interaction abnormalities
- Bacterial imbalances
- Digestive motility issues
- Stress and psychological factors Diagnosis is typically based on symptom patterns, not a specific test.
How is IBS treated?
Managing IBS often includes:
- Following a Low FODMAP Diet
- Increasing dietary fiber (where appropriate)
- Engaging in regular physical exercise
- Practicing stress management and relaxation techniques
- Using medications (antispasmodics, laxatives, or low-dose antidepressants)
- Considering psychological therapies (CBT, biofeedback, psychotherapy)
A customized approach guided by a gastroenterologist often leads to the best outcomes.
What is the best diet for managing IBS?
One of the most effective diets for IBS is the Low FODMAP Diet, which helps reduce common symptoms like gas, bloating, and irregular bowel movements. Other dietary strategies, such as eating more soluble fiber or avoiding trigger foods, may also help.
Can I drink alcohol with IBS?
It’s generally not recommended. Alcohol can irritate the gut lining, potentially triggering IBS symptoms like cramps, bloating, diarrhea, and constipation. Limiting or avoiding alcohol often leads to better symptom control.
How long does an IBS flare-up last?
IBS flare-ups can last from a few days to several weeks, depending on severity and individual health factors. Symptoms may change during the flare. Partnering with a board-certified gastroenterologist is key for monitoring symptoms and creating an effective recovery plan.
Should You Try a Low FODMAP Diet?
The Low FODMAP Diet can be life-changing for those suffering from IBS and SIBO. It helps pinpoint which foods trigger symptoms, empowering you to enjoy food again without discomfort. However, because it’s complex and restrictive, it's crucial to get medical guidance throughout the process.
- Consult a doctor or dietitian
- Follow each phase carefully
- Aim for a balanced, diverse diet long term
Finding relief from digestive issues is possible — and the Low FODMAP Diet might just be the tool that unlocks it.
Sources:
- Monash University FODMAP Research Centre. The Low FODMAP Diet. https://www.monashfodmap.com
- Johns Hopkins Medicine. The FODMAP Diet: What You Need to Know. Reviewed by Dr. Hazel Galon Veloso. https://www.hopkinsmedicine.org/health/wellness-and-prevention/fodmap-diet-what-you-need-to-know
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Irritable Bowel Syndrome. https://www.niddk.nih.gov
- PubMed. Clinical Research on the Low FODMAP Diet and IBS. https://pubmed.ncbi.nlm.nih.gov
- Cleveland Clinic. Irritable Bowel Syndrome (IBS): Symptoms, Causes & Treatment. https://my.clevelandclinic.org/health/diseases/4344-irritable-bowel-syndrome-ibs
- Harvard Health Publishing. Diet and IBS: Managing Symptoms Naturally. https://www.health.harvard.edu
- Mayo Clinic. Irritable Bowel Syndrome (IBS) – Diagnosis and Treatment. https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome